Rights campaigners have also called for G7 foreign and development ministers who are meeting in London to consider the question of overriding pharmaceutical companies’ Covid-19 patents.
Activists and many world figures argue that the step is the only way to speed up access to life-saving Covid-19 vaccines for developing nations at a time when richer countries have bought up a large part of the global supply.
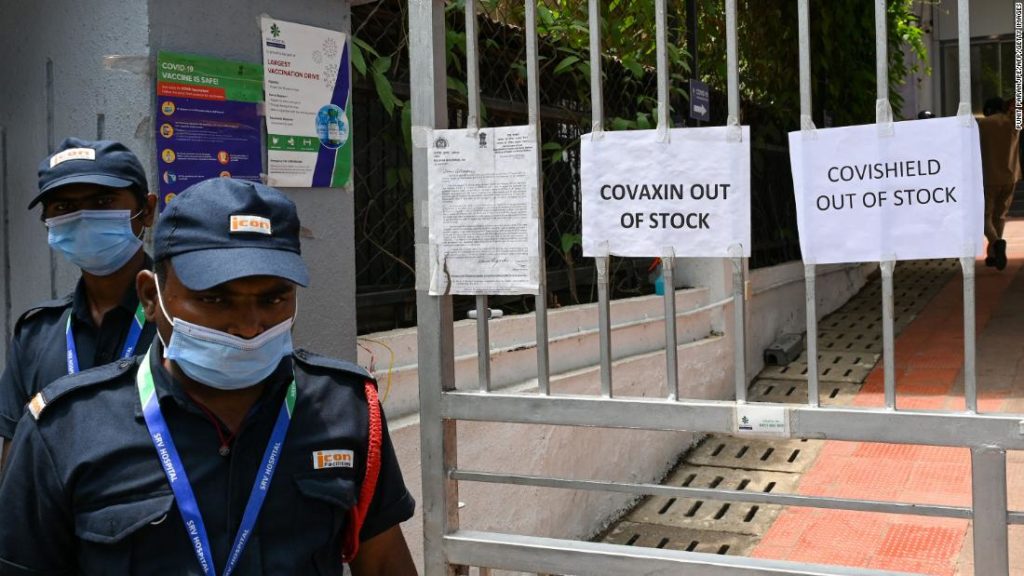
The contrast between those with vaccines and those without is clear. Western nations where vaccination programs are well advanced are now lifting many of the restrictions introduced to curb the spread of the coronavirus. Mask mandates have been eased in the US and Israel, while across much of Europe, hospitality venues are reopening and residents are planning summer vacations.
The patent-waiving proposal, first put forward by South Africa and India last October and since backed by dozens of mostly developing countries, is being considered by the WTO’s General Council following discussion last week by its Council for Trade-Related Aspects of Intellectual Property Rights (TRIPS).
The proposal calls for a waiver for all WTO members of certain provisions of the TRIPS Agreement in relation to the “prevention, containment or treatment” of Covid-19. Its proponents’ objective, according to the WTO, “is to avoid barriers to the timely access to affordable medical products including vaccines and medicines or to scaling-up of research, development, manufacturing, and supply of essential medical products.”
‘Gross failure of leadership’
Rights group Amnesty International and the People’s Vaccine Alliance urged G7 leaders Wednesday to listen to their people and ensure vaccine knowledge is shared.
“It would be a gross failure of leadership to continue blocking the sharing of life-saving technologies, and would only serve to prolong the immense pain and suffering caused by this pandemic.”
Wednesday’s WTO meeting comes a day after the chief of Pfizer said the company was expecting approximately $26 billion in revenue from its Covid-19 vaccine in 2021.
The group, led by Columbia University professors Terry McGovern and Chelsea Clinton, said the so-called TRIPS waiver would allow local manufacture of vaccines, treatments and diagnostics. “Allowing countries to manufacture locally will speed access to vaccines and treatment, prevent unnecessary deaths, and facilitate a stronger, faster economic recovery,” they wrote.
“Until vaccines, testing, and treatments are accessible to everyone everywhere we risk recurring new variants, drug resistance, and greater loss of life and suffering at home and globally.”
Legal battles
But even as public pressure grows, some experts argue that handing over the IP rights for Covid-19 vaccines won’t necessarily mean that more can be rapidly produced worldwide at large scale.
“Going back and forth, consuming time and lawyers in a legal argument about waivers — that is not the endgame. People are dying around the world and we have to get vaccines into their arms in the fastest and most efficient way possible,” he said.
Thomas Bollyky, director of the Global Health Program at the Council on Foreign Relations, told CNN on Friday that what’s really needed to scale up global manufacturing of vaccines is technology transfer. “It’s not just a matter of intellectual property. It’s also the transfer of know-how,” he said. “I don’t think there’s clear evidence that a waiver of an intellectual property is going to be the best way for that technology transfer to occur.”
Waiving patents will not work in the same way for vaccines as it has for drugs, Bollyky said. For HIV drugs, for example, manufacturers were more or less able to reverse engineer them without much help from the original developer.
“It’s very different for vaccines, where it’s really a biological process as much as a product. It’s hard to scale up manufacturing in this process for the original company, let alone another manufacturer trying to figure this out without assistance,” he said. “It requires a lot of knowledge that’s not part of the IP.”
The deal between AstraZeneca and the Serum Institute of India is a successful example of such technology transfer, Bollyky said, where the licensing of IP happened voluntarily. “The question is what can we do to facilitate more deals like the one between AstraZeneca and the Serum Institute of India to have this transfer,” he said.
Michael Head, senior research fellow in global health at the University of Southampton, in England, told CNN that increasing regional manufacturing capacity, particularly in the global south, was key — and should be a focus between pandemics.
“Sharing intellectual property during the pandemic is something that should happen but that doesn’t resolve the issues,” he said. “Manufacturing vaccines is hard. It’s hard to rapidly set up a new site with all the equipment, infrastructure, all the vaccine ingredients, with suitable staff to produce a large number of high quality vaccine products.”
“There’s only so many vaccine factories in the world and people are very serious about the safety of vaccines,” he said.
“The thing that’s holding things back in this case is not intellectual property. There’s not, like, some idle vaccine factory with regulatory approval that makes magically safe vaccines. You’ve got to do the trials on these things and every manufacturing process has to be looked at in a very careful way.”
CNN’s Nectar Gan and Maggie Fox contributed to this report.
You may also like
-
Afghanistan: Civilian casualties hit record high amid US withdrawal, UN says
-
How Taiwan is trying to defend against a cyber ‘World War III’
-
Pandemic travel news this week: Quarantine escapes and airplane disguises
-
Why would anyone trust Brexit Britain again?
-
Black fungus: A second crisis is killing survivors of India’s worst Covid wave