At dawn, market vendors busily unload fresh fruits and vegetables. Office workers fill popular eateries during their lunch breaks. As dusk falls, elderly couples descend on the city’s parks, practicing dance moves by the Yangtze River. Red lanterns have been erected around the city in anticipation of the Lunar New Year celebrations.
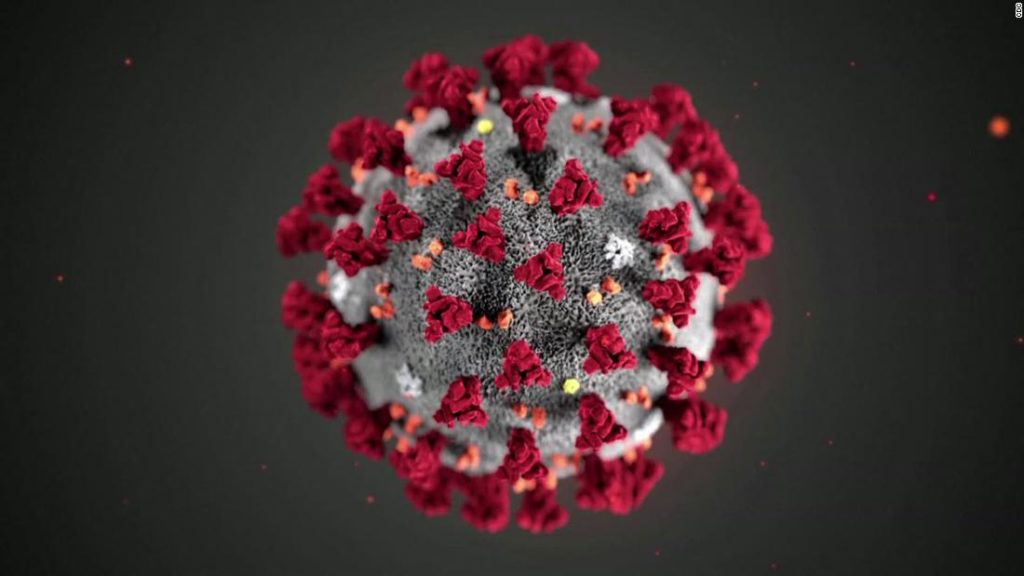
A year has passed since the central Chinese city of 11 million people was placed under the world’s first coronavirus lockdown on January 23. At least 3,869 Wuhan residents died from the virus, which has since claimed more than two million lives around the globe.
The world was stunned when flights, trains and buses leaving Wuhan were canceled, highways were blocked and people were ordered to stay in their homes, relying on officials and volunteers for daily necessities. Initially, it was difficult for patients, families and even some healthcare workers to reach hospitals.
But the Chinese government has since heralded those drastic steps as crucial to curbing the initial outbreak, and similar measures have now been enforced in countries around the world — with some cities, and even whole countries, outside China undergoing multiple lockdowns.
YOU ASKED. WE ANSWERED.
Q: Are medical masks better than cloth masks?
And while the tight weave of surgical masks offer a high level of outflowing protection — which is why they’re used by medical professionals around patients — cloth masks are more hit or miss. Their efficacy depends on the number of layers of fabric and the type of fabric used — most don’t have any sort of safety rating.
WHAT’S IMPORTANT TODAY
The megarich have already recovered from the pandemic. It may take the poor a decade to do so
Nine months. That’s how long it took the world’s top 1,000 billionaires to recoup their fortunes after the coronavirus pandemic hit.
“We stand to witness the greatest rise in inequality since records began. The deep divide between the rich and poor is proving as deadly as the virus,” said Gabriela Bucher, Oxfam’s executive director. “Rigged economies are funneling wealth to a rich elite who are riding out the pandemic in luxury, while those on the front line of the pandemic — shop assistants, health care workers, and market vendors — are struggling to pay the bills and put food on the table.”
CDC reviewing new data that suggests coronavirus variant identified in UK could be more deadly
CDC modeling shows this new strain could become the predominant variant in the United States by March. Only 195 cases of the new variant have been spotted in the US so far, according to the CDC, but public health officials believe many more cases are going undetected. Cases have been found in 22 states, the CDC says, with California and Florida detecting a particularly high number.
Reacting to the new data in an interview with CBS on Sunday, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said it should be assumed that the coronavirus variant first identified in the UK, B.1.1.7, does have the power to cause more damage, including deaths. But he also noted that both the Pfizer and Moderna Covid-19 vaccines “seem to continue to be protective against the mutant strain. It is a very minor diminution, but the cushion that you have of efficacy is so large that it’s not going to negatively impact.”
What ‘vaccine passports’ mean for your summer vacation
Some destinations — including the Seychelles, Cyprus and Romania — have already lifted quarantine requirements to visitors able to prove they’re vaccinated. Others, such as Iceland and Hungary, have opened up to people who’ve recovered from Covid-19.
This raises the prospect that proof of inoculation or immunity could be the golden ticket to rebooting travel and seems to be good news for people eager to book summer vacations after months of lockdown, particularly as vaccine rollouts gather pace.
But the concept of immunity passports remains deeply contentious, and anyone banking on them for a 2021 summer vacation could be disappointed. While there’s a strong argument that globally recognized inoculation documentation could help reconnect the planet, fears remain over what protection they actually afford, how they might be abused and what all of that means for those still awaiting jabs.
ON OUR RADAR
- The world is edging closer to a new grim milestone: 100 million cases.
- President Biden will formally reinstate Covid travel restrictions for non-US travelers from Brazil, Ireland, the United Kingdom, and much of Europe on Monday, a White House official confirmed to CNN.
- More than three dozen Capitol Police officers have tested positive for coronavirus since the Capitol riot on January 6, the union representing the Capitol Police told CNN Sunday.
- Residents of a city in northeast China have taken to social media to complain that a stringent coronavirus lockdown has left them short of food and medicine, triggering an online uproar and an apology from local officials.
- Israel will introduce a week-long ban on most incoming and outgoing flights from Monday night, in an attempt to slow the spread of new coronavirus variants.
- Mexican President Andres Manuel Lopez Obrador has become the latest world leader to test positive for the coronavirus.
- Protests against a Covid curfew in the Netherlands descended into looting and clashes with police in cities across the country on Sunday.
- The travel bubble between Australia and New Zealand has been suspended for 72 hours after the South African variant of Covid-19 was detected in a woman who had quarantined for 14 days in New Zealand.
TOP TIP
As many people postpone necessary medical care due to the pandemic, medical professionals are worried that their patients will get sick or even die from other causes.
Some 25% of Americans said that they or someone in their household had delayed medical care in the past month due to coronavirus, according to a December Kaiser Family Foundation study. An earlier report from the US Centers for Disease Control and Prevention found that 41% of Americans delayed medical care, including 12% who postponed urgent or emergency care.
TODAY’S PODCAST
“I’m optimistic that if we can have not just two vaccines, but potentially three to five vaccines rolled out, then we can get a substantial fraction of the population vaccinated during this calendar year.” — Dr. Dan Barouch
You may also like
-
UK coronavirus variant has been reported in 86 countries, WHO says
-
NASA technology can help save whale sharks says Australian marine biologist and ECOCEAN founder, Brad Norman
-
California Twentynine Palms: Explosives are missing from the nation’s largest Marine Corps base and an investigation is underway
-
Trump unhappy with his impeachment attorney’s performance, sources say
-
Lunar New Year 2021: Ushering in the Year of the Ox